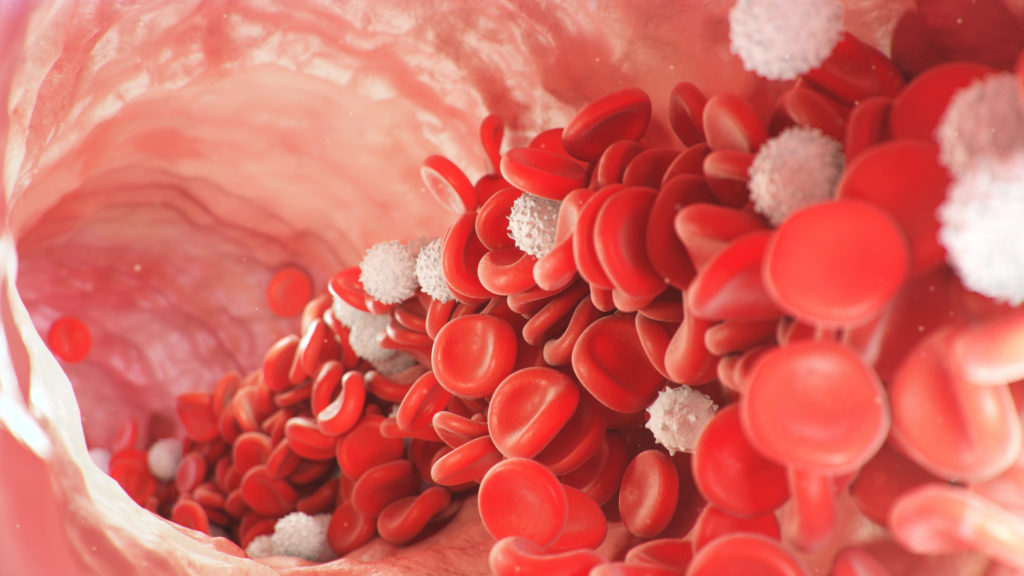
In a groundbreaking advancement for medical science, scientists have achieved a major milestone in regenerative medicine — they have successfully grown human blood cells entirely from scratch in a laboratory setting. This 2025 breakthrough discovery not only marks a significant step toward understanding early human development but also opens up promising possibilities for treating blood disorders and creating personalized therapies in the future.
Table of Contents
- Introduction
- What Was Achieved
- How the Process Works
- Why It Matters
- Technical Challenges
- Ethical Considerations
- Medical Implications and Future Possibilities
- Conclusion
1. Introduction
In a groundbreaking scientific advancement, researchers have successfully grown human blood cells from scratch in the lab. Using specialized techniques involving human stem cells, scientists have managed to replicate the earliest stages of blood development without using embryos.
This achievement could transform how we study human development, treat blood disorders, and eventually replace the need for traditional blood donations. It opens the door to patient-specific treatments and new hope for those with rare or life-threatening conditions.
2. What Was Achieved
The team developed structures in the lab that closely mimic early human embryos. These structures, built entirely from stem cells, went through stages that resemble those found in natural human development — forming layers of tissues that give rise to organs, including blood-forming systems.
What makes this accomplishment unique is that these lab-grown systems created blood stem cells, which are capable of producing all types of human blood cells. These include red blood cells (which carry oxygen), white blood cells (which fight infections), and platelets (which help blood clot).
ALSO RAED
Bone Weakness in Pakistan A Growing Public Health Challenge
Importantly, these structures do not have the capacity to form into actual embryos. They were intentionally designed to lack features such as a placenta or yolk sac, ensuring they remain scientific models and not viable organisms.
3. How the Process Works
The process begins with pluripotent stem cells, which are human cells that can transform into nearly any other cell type. These cells were cultured in lab dishes under controlled conditions that encourage them to self-organize — just as cells do in a developing embryo.
Within a few days, the cells began forming three distinct layers known as the ectoderm, mesoderm, and endoderm. These layers eventually give rise to organs and tissues. Around two weeks into the process, some of these cell structures began producing blood stem cells.
These blood stem cells are vital because they serve as the foundation for all blood components in the body. Scientists observed that the cells produced in the lab were able to mature into functional red and white blood cells — closely mirroring natural development.
4. Why It Matters
This research has several far-reaching implications:
- Understanding Development: Studying early blood formation in human embryos is extremely difficult due to ethical and practical limitations. These lab-grown models provide an ethical and accessible alternative.
- Treating Blood Disorders: Patients with diseases such as leukemia, sickle cell anemia, or bone marrow failure could benefit from lab-grown blood stem cells — especially when compatible donors are not available.
- Reducing Blood Shortages: Blood donations are critical but limited. Lab-grown blood cells, especially for rare blood types, could help fill shortages and make transfusions safer.
- Personalized Medicine: Blood stem cells grown from a patient’s own tissues would eliminate risks of rejection and complications associated with mismatched donors.
5. Technical Challenges
Despite the success, several scientific and practical challenges remain:
- Scalability: Producing a few blood cells in the lab is a remarkable achievement, but scaling up production to meet medical needs — such as transfusion quantities — remains difficult.
- Functionality: The lab-grown cells must not only look like blood cells but also function identically. This includes long-term survival in the body and proper integration into the bloodstream.
- Safety: Introducing lab-generated stem cells into patients requires rigorous safety testing to ensure no adverse effects, such as uncontrolled cell growth or immune reactions.
- Cost: Currently, growing blood cells in the lab is far more expensive than collecting blood from donors. Making this technology affordable and widely available will require further innovation.
6. Ethical Considerations
The use of stem cells and embryo-like models always brings ethical questions:
- While these lab-grown structures are not true embryos, they mimic some developmental processes. This raises concerns about how closely scientists should be allowed to replicate human life in a dish.
- In Pakistan, the National Institution of Health (NIH) plays a crucial role in overseeing biomedical research and public health initiatives.
- However, the research team specifically engineered these models to be non-viable. They cannot implant, grow into full embryos, or become living organisms.
- As the field progresses, ongoing ethical review and public discussion will be essential to ensure that science advances responsibly.
7. Medical Implications and Future Possibilities
The potential applications of this technology are extensive:
- Bone Marrow Transplants: Patients who need bone marrow transplants often face donor shortages. Lab-grown blood stem cells could serve as a life-saving alternative.
- Gene Therapy: Scientists could correct genetic mutations in lab-grown blood stem cells before reintroducing them into patients, offering potential cures for inherited blood disorders.
- Universal Blood Supply: If scientists can engineer lab-grown blood to be universally compatible, it could eliminate the need to match blood types in emergencies.
- Drug Testing and Disease Research: Lab-grown blood can also serve as a model to test new drugs and study how diseases affect human blood formation.

8. Conclusion
The ability to grow human blood cells from scratch represents a major leap forward in biomedical science. For the first time, researchers have recreated early blood development entirely in the lab — without using embryos — and generated cells that could eventually be used to treat real patients.
While hurdles like cost, safety, and scale still need to be overcome, this breakthrough offers enormous promise. It may one day lead to the end of blood shortages, open new frontiers in regenerative medicine, and deepen our understanding of human biology.
In the future, getting a blood transfusion or treating a blood disorder might not require a donor at all — just a sample of your own cells and a laboratory.